“In my community, the cost of childbirth for a male child is N25,000, and for a female child, N20,000.”
~Akin Peters from Mbaitoli LGA, Imo State.
In our ongoing mission to improve citizen participation in health sector transparency and accountability, BudgIT and CODE, with funding from the Skoll Foundation through the COVID-19 Transparency and Accountability Project (CTAP), have embarked on a strategic journey across the six geopolitical zones of Nigeria. In our previous post, we explored the Northwest region. For this post, we’ll focus on the Southeast region, a region with unique healthcare challenges and opportunities.
With its diverse population and varying socioeconomic conditions, the Southeast region needs a tailored approach to address its healthcare needs effectively. By setting the agenda for healthcare in the Southeast, we can contribute to the overall improvement of Nigeria’s healthcare system.
The Healthcare Situation in the Southeast
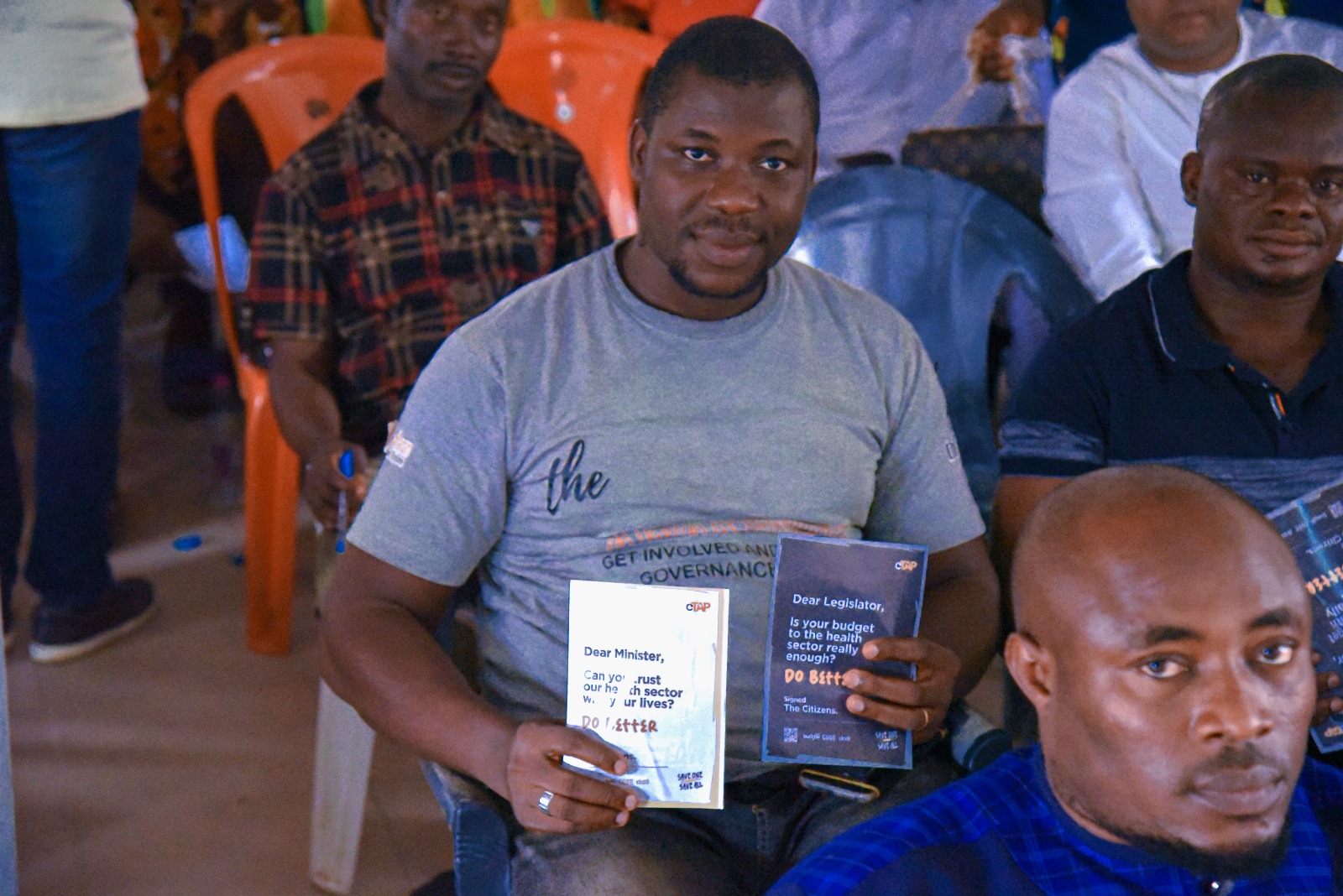
In our mission to foster a better healthcare system in Nigeria, we kickstarted the campaign with a town hall meeting that hosted about 100 participants who shared their concerns about the health sector in their communities. The meeting sparked valuable feedback, of which one of the common observations was that most PHCs in the communities were built and managed by community members, leading to neglect by the government.
While addressing developing a strategy for improving healthcare access, BudgIT’s CTAP lead, Iyanuoluwa Bolarinwa, emphasized the importance of informing the Commissioner for Health, Executive Secretaries, CMDs, Permanent Secretaries, and Director for Public Health Services about the state of healthcare in the rural areas. “As CSOs, we can only bridge the gap between citizens and the government by conveying citizens’ concerns and feedback to the relevant levels of government,” he stated.
Joy Dabirichi, an aggrieved lady from Ezeogba Emekuku LGA, shared a distressing incident involving “Nurse Eliza.” Nurse Eliza is an Igbo term for unqualified but practicing medical professionals. She told us how her baby died following a tongue operation gone wrong at a PHC. The cause of her loss came from the unavailability of an essential post-operation tool needed to control bleeding. She also shared how her neighbor’s son had a circumcision procedure at a health facility, but once again, due to Nurse Eliza’s negligence, the baby passed away in his sleep. The lack of an after-care system and the necessary drugs to sustain the child’s health contributed to this unfortunate event. These sad incidents are few among many and highlight the importance of providing necessary medical equipment in PHCs to prevent avoidable complications.
Samuel Ifeanyi, a participant from Ehime-Mbano LGA, shared an account of mistreatment when his wife needed childbirth assistance at a PHC. He was asked to get blood and pay for the procedure before providing any medical intervention. However, despite fulfilling these requirements, the staff didn’t attend to his wife promptly, resulting in severe bleeding and endangering her life. Ifeanyi said that the lack of accountability within the healthcare system calls for establishing a feedback mechanism to address such issues.
“In my community, the cost of childbirth for a male child is N25,000 and N20,000 for a female child,” said Akin Peters from Mbaitoli LGA.
The experiences shared by community members shed light on significant gaps in delivering quality healthcare services in the Southeast. Reports of negligence, inadequate after-care systems, insufficient medical equipment, and lack of accountability remain unmitigated. It is crucial to address these concerns promptly by implementing measures to enhance patient safety, improve medical resources availability, and establish an effective accountability feedback system within PHCs. Taking these steps will prevent avoidable tragedies and restore faith in the healthcare system among community members.
What were the specific needs of this region?
- Disseminating accurate information about the performance of healthcare services available in the community. ~ Akin Peters, Ihitte-meri community, Mbaitoli LGA
- Establishing proper and standard primary healthcare centers in Ezinihitte-Mbaise LGA, as the current community-owned center does not meet the required standards. ~ Immaculate, Ezinihitte-Mbaise LGA
- Addressing security, electricity, and water issues in the primary healthcare center in Ihitte-Uboma LGA, as lack of security leads to early closure of the center and hampers emergency services. ~ Udochukwu, Ihitte-Uboma LGA
- Drug provision for the PHCs. ~ Joy Dabirichi, Ezeogba Emekuku
Does the PHC staff/personnel provide satisfactory service?
“In my community of Umunoha, we have one health worker, a young lady. Despite being the only one, she consistently provides excellent service. There hasn’t been a single case of maternal mortality since she started her work.” ~ Prince Okoro, Owerri North.
“The health workers in my community receive inadequate pay, which greatly demoralizes them and results in poor service delivery. By afternoon, they have closed for the day.” ~ Chinedu, Ngokpala LGA
“There is a scarcity of staff, with only one auxiliary nurse and one experienced matron handling the workload. This heavy burden leads to subpar service and hampers efficient care delivery.” ~Samuel Ifeanyi, Ehime-Mbano LGA
How can healthcare access be improved in the communities?
- Focus on staff training, access roads, transportation, solar energy provision, adequate facilities, necessities, and accountability systems
- Provide accommodations for healthcare workers. Everyone should be trained in first-aid procedures and experiences
- Funds for facility and equipment purchase and maintenance should be channeled to the right people
- Establish channels for complaints and feedback and maintain accountability
Key Areas to Prioritize in Charting the Course for Healthcare in Southeast Nigeria
The next day, we held a round table session with key stakeholders in the health sector in the Southeast. The session addressed concerns and discussed strategies for improving healthcare services and resource management in the states. The attendees included the Imo State Commissioner for Health, Executive Secretaries, CMDs (Chief Medical Directors), Permanent Secretaries, and the Director for Public Health Services.
During the session, Iyanuoluwa Bolarinwa emphasized that field realities should precede theoretical frameworks. He stated that the importance of resource allocation based on the state’s total revenue is a crucial factor in effective healthcare provision. He suggested establishing a public finance monitoring committee with the data provided by BudgIT through this campaign. This committee should have government, civil society, and private sector representatives, which should be independent and have the authority to audit government funds and ensure they are used according to the law, and their focus should be accountability and transparency, as It is crucial to ensure the efficient use of funds
Beyond health financing, Iyanu also recommended that community champions should be set up to monitor health sector funding in the community without waiting for the government. The community champions would also serve as a tracker to give feedback to the state government.
Invaluable insights and actionable strategies on government accountability, improvement and access to healthcare facilities, non-state actors inclusion, proper governance structure in the health system, preparedness for an epidemic outbreak, and human resource management emerged from the meeting. While we, the citizens, continue to probe deeper issues plaguing Africa’s health sector, having these recommendations to guide healthcare access in Southeast Nigeria is critical. A state of emergency needs to be declared. Chief executive officers must focus on the health sector and promote collective steps toward a more equitable and accessible healthcare landscape. The discussion ended with a joint agreement that political will is crucial for health sector improvement.
Joint Round Table Recommendations
- The human resources for health in the state must develop and implement a timely policy for recruiting and appointing health personnel. This policy must focus on numbers and quality
- State governments should improve and harmonize salary and remuneration structures for health workers
- State Commissioners for Health should establish infectious disease hospitals in all the senatorial zones with functional modular laboratories and ambulance services.
- State Senates and the Houses of Representatives should set up a committee to work with the state epidemiologist in readiness for future epidemic
- State Ministries of Health, through the Commissioners for Health, should oversee agencies’ activities in the health sector
- State governments should consider CBOs, FBOs, and development partners by creating a partnership coordinating forum
- States’ National Health Insurance Authority should provide Health Insurance Schemes for formal, informal, and disabled people
- State Governments should make provisions for proper road networks and transportation peculiar to each area, like tricycles, boats, etc
- State governors should liaise with Ad-hoc staff to build equipped and standard facilities with well-trained and qualified personnel
- Health stakeholders should collaborate with CSOs to push for advocacy of accountability from the government by reminding them of their promises to the health sector
Taking collective steps towards a more equitable and accessible healthcare landscape, these recommendations will serve as a roadmap for innovative solutions and advancements in healthcare. Stay tuned for impactful outcomes.
Thank you for joining us on this journey to chart the course for healthcare in Southeast Nigeria. Together, we can make a difference and create a healthcare system that meets Nigerians’ needs.