How BudgIT is Strengthening Community Participation and Engagement.
Strengthening Community Engagement and Accountability for PHC (SCEAP) Project
In 2021, BudgIT elevated its health practice to a full-fledged unit, making this the fifth unit in the organization in addition to Budget and Research Advisory, Service Delivery Tracking, Natural Resource and Climate Governance, and Open Government and Institutional Program. Before this, BudgIT has analyzed health budgets, tracked health projects, delivered the #FixPHC project, and recently worked with Connected Development to deliver the CTAP project, which spanned COVID-19 Fund Management, Vaccine Equity, and Healthcare Accountability.
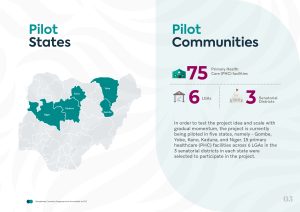
With the support of its long-standing partner, the Bill and Melinda Gates Foundation, the BudgIT Foundation is implementing the Strengthening Community Engagement and Accountability for PHC (SCEAP) project. The SCEAP project seeks to improve primary health care delivery in Nigeria through community-led advocacy and monitoring service delivery, financing, and tech infrastructure deployment to improve access and utilization of healthcare services by encouraging community advocacy and strengthening the government’s commitment to funding and delivering quality healthcare.
SCEAP empowers community actors to promote transparency and improve healthcare facilities and services through equal participation and inclusive involvement, especially for vulnerable persons and members of the target communities. This strategy will be achieved by working with the communities and other stakeholders as key drivers of change and catalysts for the project objectives.
To deliver primary healthcare services, the National Primary Health Care Development Agency (NPHCDA) has attempted to structurally embrace community engagement mechanisms by establishing different community groups and committees that would ensure community engagement becomes an integral part of primary healthcare service delivery in Nigeria.
According to the NPHCDA, structurally, every ward shall have a Ward Development Committee (WDC). At the village or community level, a Village Development Committee (VDC) shall be established. The chairpersons of the VDCs in the ward will be members of the WDC and represent their respective VDCs, bringing health facility problems beyond the capacity of the health facility to the WDC. All identified problems at the ward level are registered to the Local Government Health Authority (LGHA) for interventions and the requisite actions. However, has this worked well? Has this led to accountability or built a sense of community ownership for PHCs?
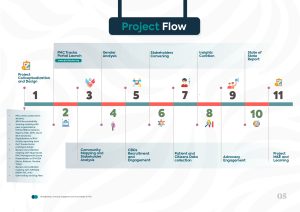
Explaining Our Project Flow
Despite the NPHCDA’s efforts, the state of the PHC system in Nigeria is shocking, as only about 20% of the over 30,000 PHC facilities across Nigeria are fully functional. The rest of the PHC facilities cannot provide essential primary healthcare services. Centers face problems including poor staffing and distribution of health workers, poor quality healthcare services, faulty infrastructure, and a lack of essential drug supply.
In 2021, while engaging in the #FixPHC campaign around the country, the SCEAP project was born. This concept was then followed by a needs assessment on how to contribute to improving PHC service delivery. BudgIT went ahead to facilitate a scoping meeting with peer organizations—White Ribbon Alliance (WRA), R4D, JDPC, Ducit Blue Solutions—where the broader idea was shared, and the peer organizations contributed their opinion on the state of PHC delivery in Nigeria and how community participation can revitalize quality service delivery.
The meeting was followed by a collaborative partnership with WRA to digitalize the reporting tools used at the PHC facilities to report to the LGAs and the State Primary HealthCare Development Agency (SPHCDA). With this, a prototype UI/UX portal was designed to aid citizens’ feedback on the state of the PHC facilities in their communities as well as on their service experience. A validation workshop was held with the former Niger SPHCDA, which had facility workers, WDCs, LGA officers, and other stakeholders in attendance.
It was followed by a review and validation workshop with the NPHCDA—NEMCHIC Unit—in Abuja to review the citizens’ feedback tool and align the questions with the agency’s strategy for tracking PHC service delivery. The final phase of the project design was a consultation visit to all the Executive Secretaries of SPHCDA in Kano, Kaduna, Gombe, Niger, and Yobe States to present the portal to them and get their feedback. Their response was integrated, and the portal was thereafter tested for bugs, which were fixed before the official public launch in July 2023.
The SCEAP Implementation Flow
Community and Stakeholder Engagement
Community ownership forms the bedrock for an effective SCEAP project in the primary healthcare system, which must include participation and engagement with the right stakeholders. It has been established that community-based organizations are the drivers of change at the community level. As such, numerous engagements championed by community-based organizations with key stakeholders at the community level, the facility, and the government were used to design the framework for the project. Convening meetings with key government bodies, NPHCDA (NEMCHIC unit ), members of the state primary healthcare board, and key focal persons at the community level while ensuring the inclusion of underrepresented gender, PLWDs, and the vulnerable populace. Information and feedback gathered from these engagements and discussions tailored and streamlined our intervention to the needs of the community.
Technology and Platform Development
A key concept of this project was centered on the community feedback mechanism. The use of technology has played a crucial role in ensuring citizens can project their feedback and concerns and proffer solutions to strengthen the PHCs in their communities. Such has necessitated developing a digital online platform dedicated to capturing responses from the community.
With this, we developed a prototype UI/UX design for a citizen feedback portal that helps citizens provide feedback on the state of the PHC facilities in their communities as well as on their service experience. With the prototype design, we had a validation workshop with the former Niger SPHCDA, which had health facility workers, WDCs, LGA officers, and others in attendance
Data Capture and Insight Development
Following the portal launch in July 2023, seven thousand pieces of feedback have been submitted, collated, and recorded on the portal to date. The data captures patient and concerned citizens’ responses, which provides a unique opportunity for their voices to be heard transparently, without any alterations. It also allows government stakeholders, development partners, and other critical stakeholders to be abreast of the PHC service delivery situation at the grassroots level. At the end of Q3 2023 (July – September 2023), across the five focus states of the SCEAP, 5,469 feedback (1,019 citizens and 4,450 patient responses) were submitted, collected, and analyzed.
Various insights have been drawn from the SCEAP project, which includes:
- Awareness of the SCEAP project has generated an increase in the awareness of the PHCs in the five focus states of implementation. The knowledge of the SCEAP project has improved the patients’ experiences at their healthcare facilities. The collaborative partnership between the community-based organizations, stakeholders, village heads/representatives, WDCs, women leaders, facility in-charges, and community members has proven instrumental in addressing healthcare challenges and enhancing service delivery.
- The SCEAP project has significantly improved relationships between the health facility and community members. These efforts have resulted in open discussions and joint problem-solving strategies between the community and the health facility. There is also an increase in service utilization at the PHCs. This is evident in increased patient turnouts that have been observed since the start of SCEAP, with a 55% increase in the number of participants visiting the PHCs weekly and a 30% increase in the monthly visits to the facilities. Additionally, specific services such as outpatient consultation/general consultation and antenatal care services have recorded a 70% increase in most facilities. The data obtained from the PAT portal has been utilized by facilities in charge to enhance service delivery.
- Key indicators to accessing care at the facility:
- Geographical location/access to the facility: Of the 4,450 patient feedback collected and analyzed, 3,426 (77%) respondents described access to their facility as easy—this can be translated to the location, walking distance, and availability of a signpost that aids visibility. On the other hand, 1,024 (23%) of persons who utilized services at the PHC described access to the facility as difficult. Kano State recorded the highest feedback from community members who described access to their facility as difficult, accounting for 377 feedback (37%), while Niger State recorded the lowest feedback, accounting for 113 feedback (11%).
- State of hygiene at the facility: A higher number of the patients (3,941—88.56%) who had visited the facilities claimed the facilities were clean as compared to the average patient (509—11.44%) population who claimed the health facilities were not clean. The claims that PHCs are clean are high across the states, indicative of the fact that hygiene has generally improved; this is also subjective.
- Condition of the waiting room: Of the total responses received from the PAT portal, 3,110 (69.88%) respondents described the waiting room of PHC in their facility as being in good condition, 1,091 (24.5%) stated that the waiting room was in a fair state and 249 (5.59%) responded that the waiting room was in poor condition.
- Basic amenities (water availability): Our observation of access to water at the PHCs under review across the five states was that a higher number of patients (84% in Kano) had access to water. In other states, there has been an improvement in the percentage of citizens with access to clean water at PHC facilities, which include Kaduna (74%), Yobe (95%), Gombe (78%), and Niger State, which showed the poorest performance with the percentage of respondents with access to clean water at 41%.
- Wait time: The report showed that only 9.6% of the patients took more than an hour to be attended to in all the primary healthcare facilities in the states, while 24% waited between 30 minutes and an hour. Most patients (about 34%) had a waiting time of 15-30 minutes. However, only 32% spent less time (15 minutes) before being attended to.
- Availability of prescribed medications: A total of 842 (18.9%) responses attested to the availability of drugs at the PHC facilities, while 3,608 (81%) patient feedback revealed the non-availability of drugs at the PHCs. Hence, there is a need to mobilize more advocacies for the supply of drugs to health facilities to ensure their availability.
The recurrent needs among healthcare facilities include the need for additional manpower to meet the increasing patient load and curb the mass exodus of healthcare at the facilities, the need to renovate some facilities, especially in Niger and Kano States, while prioritizing the provision of medical supplies and equipment to aid service delivery at the facilities.
The cumulative aggregate of 50% of the community members rated the health workers positively, noting improvements in service delivery following the SCEAP project. They also reported a positive change in the behavior and practices of the healthcare providers, including a positive relationship toward the health seekers. However, the condition of the health facilities was a concern, with the majority of the feedback requesting urgent renovation of the PHC facilities, the provision of basic amenities like water and electricity, ensuring availability and affordability of medications and drugs, and security personnel in areas prone to communal clashes, kidnapping, banditry, and insurgency, especially in hard-to-reach communities.
There are inadequacies in the staffing capacities at the PHCs, which has led to dual responsibilities and duties, as such records and data are not properly managed in most facilities. Improving the staffing bandwidths at the PHCs will improve record-keeping and data management. However, some PHCs have been successfully collating and updating their data. To do this, they take records before rendering services to patients, hence ensuring correct and updated records.
Closed Feedback Loops
Advocacy and engagement with the government following feedback generated on the PAT portal were crucial in ensuring government involvement in the SCEAP project, especially at the state healthcare level (SPHCDA). In September 2023, the first state convening meeting held across the five implementing states provided an avenue for all stakeholders to assess their states’ performance (using the health indicators profiled on the portal), discuss their challenges, and dialogue on the next steps. A quarterly progress report is shared with the ES of the respective implementing state, providing an opportunity for government stakeholders, development partners, and other critical stakeholders to be abreast of the reality of PHC service delivery at the grassroots level.
The SECAP project also recorded engagement at the community level involving the key stakeholders (WDCs and facility representatives with a high emphasis on gender inclusion, PLWDs, and the vulnerable population). This has resulted in activation and coordination between the already established community stakeholders and the government. This act of communication has witnessed additional manpower in some facilities in Gombe, Kaduna, and Yobe State, respectively, while addressing security challenges in Kaduna and Niger State.
The Way Forward
The SCEAP project has managed to create an active link between the communities and stakeholders, facilitating a system where issues are promptly identified and addressed. The findings from the project are ongoing to improve the standard of healthcare in these areas, and the need for continued investment is crucial to its sustainability.
As part of the measures to ensure Universal Health Coverage (UHC), the collaborative efforts between government stakeholders, the community, and civic society play a crucial role in strengthening the primary healthcare system. Community participation tailored towards sensitization and advocacy is the key to ownership at the grassroots level. Using the responses generated on the PAT Tracka Platform for sensitization, advocacy, and engagement at the community and government levels (LGAs and state levels), especially regarding the state of the infrastructure and human resources, are the next steps to engage the government actively.
While the SCEAP project has shown promising results, additional support is needed to raise awareness and increase the number of health workers while developing a reward system to encourage the health staff and maximize the positive impact on community engagement and healthcare outcomes.



